Written by Lucienne Ide, MD, PhD | Founder of Rimidi
In medicine, we often talk about meeting a patient where they are. Usually, this is in reference to their health literacy levels or their readiness to follow a treatment plan. It’s more challenging to physically meet patients where they are—especially those in rural communities where there is poverty, with remote locations and fewer local doctors. A quarter of Americans who live in rural areas have to drive an average of 34 minutes to reach the nearest acute-care facility, severely limiting their access to care in these areas. These barriers to care affect patient outcomes and, ultimately, overall quality of life.
Connectivity is Essential to Care
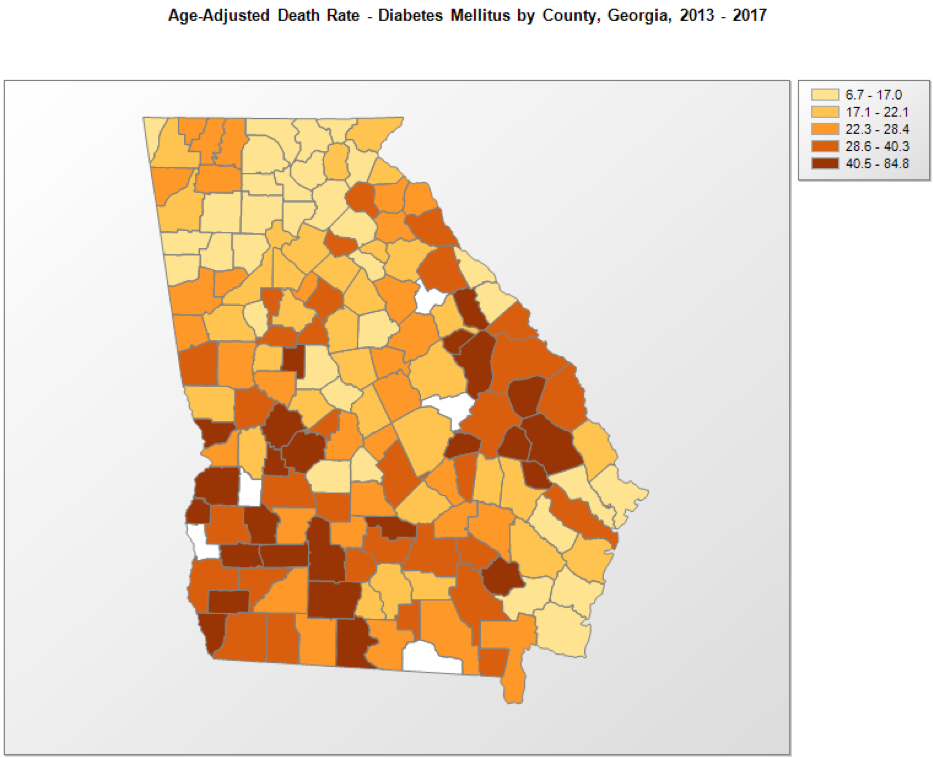
Lack of access to care causes people who live in rural communities to be disproportionately affected by chronic diseases, like diabetes and heart disease, compared to urban areas. In fact, the prevalence of diabetes in the country’s least-connected rural communities is 41% higher than the national average. In my own state of Georgia, diabetes prevalence is 3.4 times higher in households with incomes less than $15,000 and 2.4 times higher in adults who did not graduate from high school. Even more troubling, the likelihood of dying from diabetes is higher for those who live in rural parts of the state.
The recent emphasis on telehealth and mobile health technologies is promising, but there are still many challenges to overcome. Most notably, the same rural areas affected by higher chronic conditions and mortality rates are also less likely to have reliable broadband access, leaving communities without access to the telehealth services that could save lives.Studies show that patients in an intensive care unit equipped with telehealth services were discharged 20% quicker and saw a 26% lower mortality rate than those in one without telehealth capabilities. In order to improve the quality of life and overall health of rural Americans, it is essential that these areas have a reliable broadband connection.
Working with the FCC
Thankfully, the Federal Communications Commission (FCC) is aware of the broadband challenges and the impact on rural healthcare if we solve the issue. A few weeks ago, the Rimidi team sat down with FCC Chairman Ajit Pai and former Atlanta Hawks basketball star and type 2 diabetes awareness advocate, Dominique Wilkins. We explained the challenges we face at Rimidi in pursuit of achieving better patient outcomes in rural areas, particularly, the need for improved broadband infrastructure in rural areas so patients can better access their telehealth services.
During this visit, we learned that the FCC is keenly focused on getting broadband to rural areas for connected health capabilities. Last summer, the FCC proposed a $100 million Connected Care Pilot Program to enhance the advancements made in the telehealth industry, eventually leading to significant cost savings and improved patient outcomes. Another program by the FCC focuses specifically on rural health care, hopefully raising $400 million annually in order to promote broadband deployment. However, more must be done to ensure that rural Americans don’t fall on the wrong side of the digital health divide.
The good news is that unlicensed spectrum via TV white spaces to make up the difference in an extremely cost-effective way to deliver broadband to hard-to-reach rural areas. Basically, TV white spaces refers to the unused TV channels between the active ones in the VHF and UHF spectrum bands. This technology can assist the FCC in its goal to connect rural Americans by serving as a virtually untapped resource to expand a wireless broadband signal’s reach. TV white space signals can also traverse difficult terrains (e.g., mountains) with relative ease as compared to its wireline or cellular counterparts. Although the FCC has made some great strides in opening some of these bands for unlicensed broadband use, we need them to rule on relevant proceedings for this possibility to be fully realized, which helps us to be better positioned to provide our service to more patients living in rural areas.
Improving Outcomes
After working as a scientist, a venture capitalist, and training as a clinician, I left the ranks of clinical medicine to drive innovation in the healthcare industry with Rimidi. Rimidi is a cloud-based software solution that enables personalized management of chronic cardiometabolic conditions across populations, including heart failure, type 2 diabetes, and fatty liver disease. We integrate patient-generated health data from connected devices (like connected glucometers or blood pressure cuffs) with patient data in a health system’s electronic medical record, giving clinicians a more complete view of each patient’s health while working within their existing workflow.
The vision of personalized medicine depends on the ability for providers to incorporate patient-generated data into their clinical decision-making, and incorporating this data is dependent on the patient being connected. An astounding 24 million Americans do not have access to internet and 146 million Americans can barely afford a low-priced broadband plan, causing the health disparity to rise even more with lack of broadband access presenting itself as yet another barrier to better health. According to the FCC, a third of Americans in rural areas don’t have internet connections that meet the minimum definition of broadband service needed to use a telehealth platform such as ours.
I decided to start Rimidi based on the simple idea that we could do better in healthcare, as physicians, as administrators and leaders, and as politicians. Closing the disparity in broadband access is certainly a step in the right direction.